Estrogens are pivotal regulators of brain function, exerting profound effects from early embryonic development to aging. Extensive experimental evidence underscores the multifaceted protective roles of estrogens on neurons and neurotransmitter systems, particularly in the context of Alzheimer’s Disease (AD). Studies have consistently revealed a greater risk of Alzheimer’s Disease (AD) development in women compared to men, with postmenopausal women exhibiting heightened susceptibility. This connection between hormone levels and long-term estrogen deprivation highlights the significance of estrogen signaling in Alzheimer’s Disease (AD) progression.
The pathogenesis (the process by which a disease develops) of Alzheimer’s begins with the breakdown of the amyloid precursor proteins to produce beta-amyloid, which accumulates around the cerebral blood vessels, forming amyloid plaques. Amyloid plaques weaken the vessel walls, leading to intracranial hemorrhage. Besides this, beta-amyloid also has a neurotoxic effect on the brain, destroying neurons and causing atrophy of the cortex. In addition, beta-amyloid accumulation in the nucleus of the meynert (forebrain) causes the loss of acetylcholine, the neurotransmitter essential for memory and learning. As the disease progresses, the tau protein, a naturally occurring protein bound to microtubules and involved in neuronal transmission, detach from the microtubules and form clumps inside neurons, inhibiting signal transduction. Free radical-mediated oxidative damage is also involved in the development of neurodegeneration in Alzheimer’s.
Patients with dementia experience a progressive decline in neurocognitive function, beginning with short-term memory loss that progresses to long-term memory loss and the inability to perform everyday activities, leading ultimately to death. There is currently no cure for dementia, so preventing or slowing the disease’s progression is paramount. Accordingly, researchers have studied the role of estrogen as a neuroprotective agent. Estrogen prevents dementia by augmenting hippocampal and prefrontal cortex function in the brain, reducing neuroinflammation, preventing degradation of estrogen receptors, decreasing oxidative damage to the brain, and increasing cholinergic (nerve cells where acetylcholine acts as a neurotransmitter) serotonergic (serotonin mediated) function.
According to the WINDOW PHASE HYPOTHESIS, estrogen’s effect on preventing dementia is more pronounced if therapy is started early, during the first five years of menopause.
In women, estrogen is involved in the development of the reproductive system and contributes to both primary and secondary sexual characteristics. Studies also show that it exerts a neuroprotective effect. Interestingly, studies on the use of Hormone Replacement Therapy (HRT) in postmenopausal women suggest a protective effect against cognitive decline, specifically maintenance of brain tissue integrity with HRT. They suggest that supplemental estrogen protects cognition in multiple ways e.g. by promoting cholinergic activity; protecting the brain from toxic insult; stimulating neuron synthesis, and reducing deposition and enhancing the clearance of β-amyloid (the main constituent of the amyloid plaques seen in Alzheimer’s disease).
The effects of HRT can be complex; long term estrogen therapy appears to be beneficial in slowing the progression of Alzheimer’s but it is usually combined with a synthetic progestin in women with an intact uterus to prevent endometrial (lining of the uterus) cancer. Synthetic progestins can suppress memory, especially in older women. Research suggests that unlike synthetic progestins natural progesterone does not have this negative impact on memory and furthermore, it should be administered vaginally so that it concentrates in the uterus and only a small fraction enters the systemic circulation and reaches the brain. This is of course unnecessary in women who have had a hysterectomy where HRT consists solely of estrogen, as there is no need for an endometrial protective effect.
The choice of the route of administration of estrogen can play a significant role in avoiding potential negative cardiovascular effects. Oral estrogen increases the risk of blood clots compared to transdermal (patches or gels) estrogen. All drugs or hormones taken orally must pass through the liver before they reach the systemic circulation. When oral estrogen passes through the liver it undergoes changes that lead to increased levels of clotting factors and decreased levels of antithrombin III (a naturally occurring anticoagulant) increasing the risk of venous thromboembolism (blood clot). On the other-hand transdermal estrogen bypasses the liver, reducing the risk of blood clots.
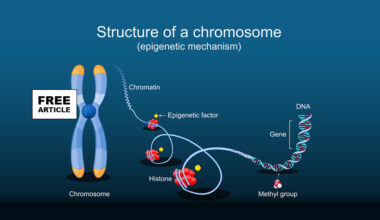
Brain mitochondria, the powerhouse of cells, are involved in brain energy production, oxidative stress regulation, and apoptosis (cell death). Oxidative stress accelerates with aging, accumulating reactive oxygen species (ROS) that damage lipids, proteins, and mitochondrial DNA. Mitochondrial dysfunction from oxidative stress is the first pathologic change observed in the aging brain and many neurodegenerative diseases, including Alzheimer’s. Protein studies have highlighted the role of estrogen in mitochondrial expression. Long-term estrogen deficiency in postmenopausal women leads not only to altered Estrogen Receptor (ER) expression but also to exacerbated oxidative stress in the brain, giving rise to mitochondrial impairment and cholinergic degeneration, ending eventually in reactive gliosis (a scaring process in the brain characterized by an increase in the number and size of supporting glial cells in response to injury). Correspondingly, brain mitochondria are believed to be the targets for estrogen’s neuroprotective effect.
Multiple studies indicate that there is optimal period, or rather, a window of opportunity – WINDOW PHASE HYPOTHESIS – for prescribing estrogen therapy that results in better cognitive outcomes in post-menopausal women. This period is hypothesized to be during perimenopause or right after menopause, specifically during the first five years. There are several factors that could explain this, based on the results of various observational and interventional clinical trials. First, a long premenopausal phase when significant levels of estrogen continue to be naturally produced is associated with greater cognitive function and a decreased risk of Alzheimer’s Disease (AD). The risk of AD is reduced by 0.5% for every additional month of estrogen exposure before menopause. Second, there is a reduction in the number and affinity of Estrogen Receptors (ERs), especially Estrogen Receptor alpha (ERα,) with the prolongation of the hypoestrogenic phase associated with menopause. Patients with AD exhibit a straight-line declining relationship between the number of ERα and cognitive function, which further supports the idea of ‘ERα degradation and a less-than-optimal response to hormone therapy, or no response when therapy is initiated after the 5-year window of opportunity. Starting estrogen later in life (e.g. age 65+) does not appear to help.
Researchers have not defined the optimal length of estrogen therapy to delay or prevent the onset of Alsheimer’s disease. However, current practice suggests it should be between 5 and 7 years. Further research is need to know the optimal length of therapy for the prevention of Alsheimer’s disease.
All signaling pathways require enzymes and/or co-factors, and those require vitamins. Accordingly, correcting vitamin deficiencies before initiating estrogen therapy is pivotal.
Sources
https://pmc.ncbi.nlm.nih.gov/articles/PMC10480684/
https://www.sciencedirect.com/science/article/abs/pii/S0960076004004157