Multiple sclerosis (MS) is a chronic autoimmune disease where the body’s immune system mistakenly attacks the myelin sheath, the protective covering around nerve fibers in the central nervous system (brain and spinal cord). This damage slows or blocks nerve signals, leading to a wide range of symptoms. Multiple sclerosis is significantly more common in women. Women are up to three times more likely to develop MS with the most common type, relapsing-remitting MS, being particularly prevalent among women. MS is typically diagnosed between the ages of 20 and 40.
MS can be defined as an autoimmune demyelinating neurodegenerative disorder in which immune cells T-cells and B-cells mistakenly target myelin. T-cells and B-cells are both types of lymphocytes which are white blood cells crucial for the adaptive immune response. Loss of the myelin sheath disrupts nerve conduction causing the neurological symptoms. Over time, axonal damage and brain atrophy can occur.
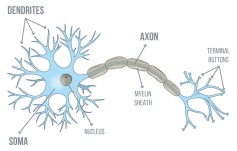
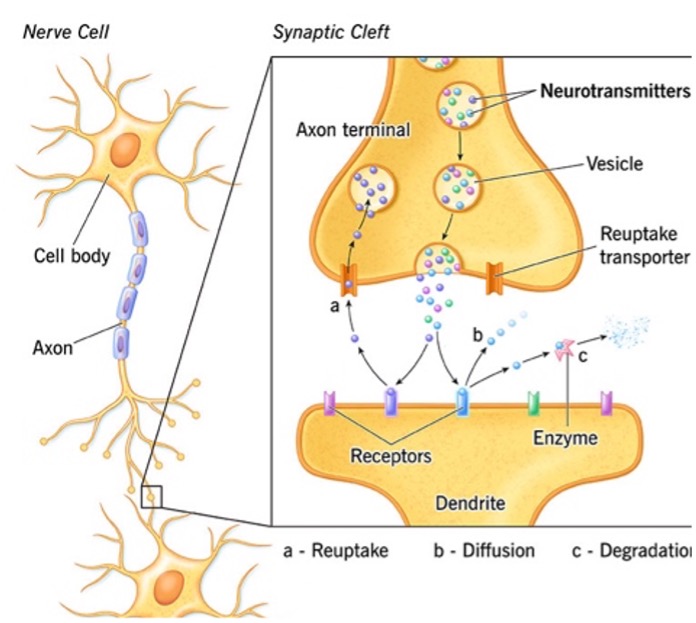
Axons are the long threadlike part of the nerve cell, neuron, along which impulses are conducted from the cell body to other neurons. For clarity, a neuron is the basic unit of the nervous system and has three parts: the dendrites, the cell body (soma) and the axon. Dendrites receive signals from other neurons, the soma integrates these signals, and the axon transmits signals to other neurons.
The juncture between one nerve’s axon to a dendrite of the adjoining neuron is called a synapse. The axon releases a neurotransmitter such as acetylcholine or norepinephrine to communicate with the adjoining dendrite. Synapses also allow neurons to communicate with muscle cells and glands.
MS is characterized by Inflammation, demyelination, neuronal loss, and gliosis. Myelin is a fatty substance that forms a sheath around nerve fibers, primarily in the brain and spinal cord. Gliosis is a reactive process where glial cell particularly astrocytes proliferate and become larger in response to the disease. Myelinated axons in the CNS are the primary target of MS attacks, which can cause varying degrees of damage to both myelin and the underlying axons.
Symptomatic periods in MS are “separated in time and space,” meaning that they may appear years or months apart and upset different anatomical locations of the brain. Symptoms can vary widely among patients, with some experiencing cognitive challenges, weakness of limbs, ataxia, visual disturbances, anxiety, or depression. It is imperative to note that physical or mental disability in MS may occur even in the absence of clinical exacerbations. The duration of an MS attack also known as relapse or flare-up can vary significantly, typically lasting from a few days to several weeks and in some cases even months. Most attacks develop over hours or days, peak within a few days, and then gradually resolve over weeks or months.
Historically, MS has been considered an organ-specific T-cell mediated autoimmune disorder but now this dogma is being challenged by the success of B-cells targeted therapies.
Types of MS
There are several forms:
- Relapsing-Remitting MS (RRMS):
Most common (~85% at diagnosis). Symptoms flare (relapse) and then improve (remit). - Secondary Progressive MS (SPMS):
Often follows RRMS. Gradual worsening of symptoms over time, with or without relapses. - Primary Progressive MS (PPMS):
Steady worsening from the start, without clear relapses. - Progressive-Relapsing MS (PRMS):
Rare. Progressive disease with occasional relapses.
Multiple factors contribute to the risk of MS These factors include environmental factors, genetic associations, and immune factors.
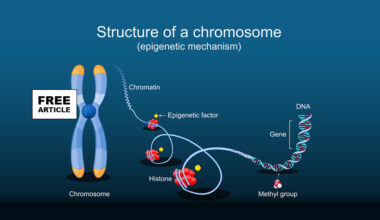
Genetics have an important role in the development of MS. Genetic factors account for 30% of MS cases. It has been shown that patients having biological relatives suffering from MS have a heightened risk of MS. First-degree relatives account for 2–4% of risk; 2% for parents and child, 20–30% for identical twins, 5% for fraternal twins, and 1% for the general population.
Environmental factors appear to be the main contributors to MS development. For example, latitudinal gradients have been extensively studied over the years, correlating with the prevalence of MS. This latitudinal gradient of MS is strongly related to ultraviolet B (UVB) exposure and vitamin D production. UVB rays are crucial for vitamin D production in the skin. Vitamin D is linked to MS, with low levels potentially increasing the risk of developing the disease and influencing disease activity. Low vitamin D intake, less outdoor activity, and a genetic predisposition to low vitamin D contribute to MS development.
Research indicates that childhood and adolescent obesity is linked to elevated levels of C-reactive proteins, leptin, and interleukin-6 (IL-6), promoting a pro-inflammatory state that influences the pathogenesis of MS, i.e. the way in which the disease develops. Tobacco contains high levels of free radicals and negatively affects the immune system. Smokers exhibit elevated levels of pro-inflammatory cytokines such as IL-6, fibrinogen, C-reactive protein, and other inflammatory markers that contribute to the autoimmunity seen in MS.
Epstein Barr Virus, EBV infection also increases the risk of MS. More than 99% of patients with MS have EBV antibodies that indicate a prior EBV infection. Recent studies have now strongly suggested the involvement of EBV infection in subsequent MS development. A meta-analysis showed that EBV infection was associated with a 2.6-fold increase in risk for developing MS. EBV is part of the human herpes virus family (HSV). It is an enveloped virus with a double-stranded DNA genome that codes for 85 proteins and several non-coding RNAs. The virus is transmitted through saliva and infects the epithelial cells in the pharynx. Once released from these epithelial cells, it can infect B-cells in the underlying tissues. Depending on the environment and the host’s immune response, the virus may either propagate or enter a latent state. The mechanism by which EBV contributes to the development of MS is not yet fully understood. However, research has identified several pathways through which EBV-infected B cells may promote MS development. Persistent EBV infection can lead to immune tolerance and trigger autoimmunity. This persistent infection causes dysregulation of B cells and the emergence of autoreactive B cells.
EBV proteins, such as Epstein bar virus nuclear antigen-1 (EBNA1), share structural similarities with myelin basic proteins (MBP), resulting in molecular mimicry. This mimicry can mislead the immune system into attacking myelin through a cross-reactive immune response.
The inability to effectively clear infected B cells can lead to damage to the axon and myelin sheath. Continuous EBV infection might also stimulate the response of CD8+ T cells, which can result in central nervous system injury.
Treatment
MS has no cure yet, but treatments aim to:
Reduce relapses, Slow disease progression and Manage symptoms
- Disease-Modifying Therapies (DMTs)
They prevent relapses and lesions.
Most effective early in relapsing forms (RRMS).
Common DMTs:
Injectable drugs:
- Interferon beta-1a or beta-1b (e.g., Avonex, Rebif, Betaseron, Extavia)
- Glatiramer acetate (Copaxone) — shifts immune response to protective type.
Oral drugs:
- Fingolimod, Siponimod, Ozanimod, Dimethyl fumarate, Teriflunomide
Infused monoclonal antibodies:
- Natalizumab (Tysabri) — highly effective but risk of PML (a brain infection).
- Ocrelizumab (Ocrevus) — approved also for Primary Progressive MS.
- Ofatumumab (Kesimpta) — self-injected.
- Alemtuzumab (Lemtrada) — reserved for aggressive MS.
When flare-ups occur:
High-dose corticosteroids (e.g., IV methylprednisolone) to reduce inflammation quickly
Plasma exchange (PLEX) — if not responding to steroids