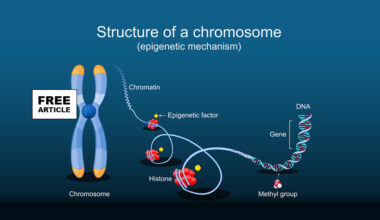
During pregnancy, there is a physiological exchange between mother and fetus through the placenta This transplacental traffic can be unidirectional or bidirectional. The unidirectional transfer involves nutrients, water, electrolytes, oxygen, hormones, and immunoglobulins being transferred from the mother to the fetus and carbon dioxide and catabolism products from the fetus being transferred to the mother. Bidirectional traffic consists of maternal-fetal exchanges of cells and genetic material such as DNA.
Microchimerism is the presence of cells from one individual residing in another genetically distinct individual. Pregnancy is the main example of naturally occurring microchimerism exemplified by transplacental bi-directional cell trafficking between mother and fetus. During pregnancy, there are two types of feto-maternal microchimerisms: fetal microchimerism (FMc) and maternal microchimerism (MMc). FMc is defined as the presence and persistence of fetal cells in maternal tissues, while maternal microchimerism (MMc) is defined as the presence and maintenance of maternal cells in fetal tissues. The fetal cells, which originate from the developing embryo and cross the placenta during gestation, can integrate into various maternal tissues and organs. Remarkably, they have been detected years, even decades, postpartum. Microchimerism may also occur other than the transfer of cells between the mother and the fetus. An exchange of cells can also take place between twins in the uterus. This transplacental maternal-fetal cell transfer is asymmetric, with a higher fetal cell trafficking to the maternal body.
Fetal cells cross the placental barrier and enter the maternal circulation, where they can survive, migrate, and integrate into different maternal tissues. Fetal microchimerism (FMc ) has been detected in various organs such as the bone marrow, pituitary gland, appendix, liver, brain, heart, lung, kidney, thyroid, lymph nodes, and pancreas. Once FMc has been established in the maternal organs, they differentiate into cell lines thanks to their high multiline capacity and stem cell like plasticity
Fetal microchimerism functions as a two-edged sword; it has been associated with both beneficial and adverse effects on maternal health. Fetal microchimerism has been shown to have several beneficial effects on maternal health. These fetal-derived cells can also migrate to sites of tissue injury, inflammation, or degeneration, where they may contribute to tissue repair and regeneration due to their stem cell-like properties. For example, in cases of maternal tissue damage, such as heart injury or skeletal muscle injury, fetal cells have been observed to assist in the healing processes by differentiating into specialized cell types, thereby promoting tissue repair and restoring function. Additionally, FMc microchimerism may help enhance immune regulation, promoting tolerance and reducing the severity of autoimmune responses in certain contexts.
This phenomenon could serve an evolutionary advantage by providing the mother with a cellular memory of fetal antigens, potentially aiding in immune adaptability. In lung cancer, primiparous and multiparous women have a better prognosis than nulliparous women and men, suggesting that FMc could suppress maternal tumor development. FMc presence is also related to a lower risk of breast cancer. Overall, current research suggests that maternal microchimerism plays a beneficial role in tissue maintenance and repair, contributing positively to maternal healing and health following pregnancy, and represents a fascinating form of natural biological cooperation between mother and fetus.
Conversely, fetal microchimerism is also implicated in autoimmune conditions, as the presence of foreign fetal cells might trigger immune responses, contributing to diseases like systemic lupus erythematosus (SLE) or autoimmune thyroiditis. Other studies have reported a higher proportion of fetal cells in women with cancer (specifically colon cancer) women with autoimmune diseases such as systemic sclerosis, rheumatoid arthritis, Sjogren syndrome and with non-autoimmune pathologies such as hepatitis C. Research into microchimerism is ongoing, aiming to understand the complex interactions between these cells and maternal physiology.
In summary, on the one hand, fetal microchimerism (FMc) could be a source of progenitor cells with a beneficial effect on the mother’s health by intervening in tissue repair, angiogenesis, or neurogenesis. On the other hand, FMc might have a detrimental function by activating the immune response and contributing to autoimmune diseases. By, shedding light on this intricate biological exchange, scientists hope to uncover how fetal cells influence long-term health outcomes for mothers and potentially harness this natural phenomenon for therapeutic purposes.