Immunization has become a vital part of public health and disease prevention, and yet, it remains a controversial topic in our society today. Diseases that were once responsible for significant morbidity and mortality have now become all but eradicated, thanks to the introduction of vaccines. Immunization has contributed to increased life expectancy and improved quality of life.
The first vaccine is credited to Edward Jenner, who in 1796 inoculated a 13-year-old boy with the virus responsible for cowpox, and he demonstrated immunity to smallpox. The first smallpox vaccine was created in 1798 using that premise. Over the following centuries, and leading up to the present day, vaccine technology has improved, and vaccines for many illnesses have been developed. In 1979, global eradication of smallpox was achieved thanks to immunization.
A vaccine is a pharmacologic compound that improves a person’s immune response to a particular disease. When a disease-causing bacterium or virus invades the human body, the immune system recognizes the material as foreign, usually by detecting specific protein portions of the invading organism, known as antigens. Vaccines contain a form of the disease-causing agent, whether it be a weakened or killed form of the microbe itself, an inactivated version of its toxins, or a protein from the surface of the microbe. By introducing a form of the organism, the vaccine presents the antigen to the immune system, allowing it to recognize the antigen as foreign and develop antibodies and memory T-lymphocytes against those antigens. This allows a more rapid and robust immune response should the body be exposed to the same organism in the future. In the absence of vaccination, the first exposure to the natural organism may prove fatal before the immune system can mount a sufficient immune response.
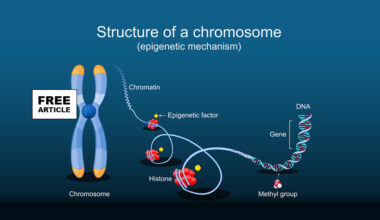
Vaccines affect the immune system, primarily through B-lymphocytes and T-lymphocytes (white blood cells). Before exposure, the immune system contains naïve B-lymphocytes and T-lymphocytes, each having the potential to respond to a unique antigen. In addition, many antigens require a combined response of both B-lymphocytes and T-lymphocytes. This form of immunity is termed T-cell-dependent. Less commonly, an antigen causes stimulation of B-lymphocytes and antibody production without the help of T-lymphocytes. This form of immunity is termed T-cell-independent.
The vaccine introduces the antigen to begin the process, which stimulates the initiation of the immune response. Initially, the foreign material is phagocytized, ingested and broken down by macrophages, a type of white blood cell. Then, the resultant peptides created by the breakdown of the protein material are sent to the surface of the macrophage cell, where it is displayed. These protein antigens are displayed by molecules called major histocompatibility complexes (MHC), which exist in 2 forms: I or II (MHC-I or MHC-II). The presentation of the antigen stimulates the secretion of several inflammatory mediators, including cytokines and various interferons, which stimulate a further response.
mRNA vaccines such as the Covid vaccine contain messenger RNA wrapped in a lipid nanoparticle to protect it. The mRNA instructs cells to make a harmless piece of the virus, usually a spike protein. (Spike proteins allow viruses to penetrate host cells and cause infection.) Ribosomes in your cells read the mRNA instructions and build the viral proteins. Your cell displays this protein fragment on their surface via the major histocompatibility complexes (MHC) in the same way as traditional vaccines.
In T-cell-dependent immunity, so-called T-helper cells recognize the antigen and stimulate the corresponding B-lymphocytes to proliferate and produce antibodies. As the B-lymphocytes proliferate, they also differentiate into antibody-forming cells called plasma cells. The antibodies produced have various functions, the most important of which include those that inactivate soluble protein toxins (antitoxins), those that facilitate intracellular digestion of bacteria by damaging the bacterial membrane (lysins), those that prevent reproduction of pathogenic viruses (neutralizing antibodies), and those that prevent bacterial adhesion to mucosal surfaces (antiadhesion). In response to vaccines, antibodies are produced called immunoglobulins primarily immunoglobulin (Ig), first IgM, with a gradual switch to IgG in the following weeks. Vaccines can be classified as live attenuated vaccines, killed or inactivated vaccines, subunits, or toxoids (tetanus).
Childhood vaccinations are indicated for the prevention of a multitude of viral and bacterial infections and their sequelae. Specific vaccination recommendations for children vary by region, as exposure to diseases varies by region. Current recommendations for adult vaccination include a yearly influenza vaccine and tetanus-diphtheria every 10 years, with tetanus-diphtheria-acellular-pertussis at least once in adulthood. The addition of acellular pertussis once during adulthood is intended to prevent the transmission of whooping cough to young children or those unable to be vaccinated. For those adults born after 1956 who didn’t receive measles, mumps, rubella vaccinations, or varicella vaccinations as children, these vaccinations are recommended in adulthood. Human papillomavirus, hepatitis A, and hepatitis B vaccines are also recommended in adulthood. The meningococcal vaccine is recommended for adults at high risk, such as those living in close quarters (college students living in dorms, military personnel living in barracks). Pneumococcal vaccination is also recommended for high-risk adults, such as those with pre-existing pulmonary diseases like chronic obstructive pulmonary disease.
Passive immunization is indicated in patients who cannot form antibodies, such as those who are immunocompromised. Passive immunization is a type of immunity where preformed antibodies are transferred to a person to provide immediate but temporary protection against a specific pathogen. It is also indicated when the disease may develop before active immunity can develop antibodies, such as in a patient exposed to rabies.
Contraindications to immunization are rare. The primary contraindication is an allergy to a vaccine or a component of the vaccine. Patients with a history of a compromised immune system, such as in acquired immunodeficiency syndrome AIDS or another immune deficiency, should use caution when vaccinating with a live attenuated vaccine. Live attenuated vaccines should not be given to a pregnant woman unless there is an immediate risk (such as a polio epidemic), as the live vaccines have the potential to infect the fetus. Severely immunocompromised persons generally should not be administered live vaccines. Common examples of live attenuated vaccines measles, mumps, rubella, yellow fever, varicella (shingles).
Most vaccines carry a small risk of adverse symptoms following administration, including fever, fatigue, and myalgias (muscle pain). These symptoms are caused by the immune response being mounted against the antigen introduced by the vaccine and usually last a day or 2. Swelling and redness may occur at the injection site, and localized muscle soreness may also occur. More serious complications are possible, though extremely rare. Anaphylaxis may occur in response to a vaccine or one of its ingredients. Another very rare complication of vaccination is Guillain-Barre Syndrome, a potentially life-threatening condition affecting the peripheral nervous system.
Vaccination is vital to public health. Disease prevention has been proven to prolong life expectancy and improve quality of life. As antivaccination movements gain traction, diseases once thought to be eradicated or nearly eradicated have had significant outbreaks. Unfortunately, preventive measures such as vaccines are often overlooked by primary care providers and patients. For children, parents often do not know the appropriate schedule for vaccines, and therefore are often unaware of when their children are behind on vaccinations. Another common reason for missed vaccination is missed appointments for various reasons. Patient recall and reminder systems have been created and have shown significant improvement in increasing vaccination compliance rates.
Sources