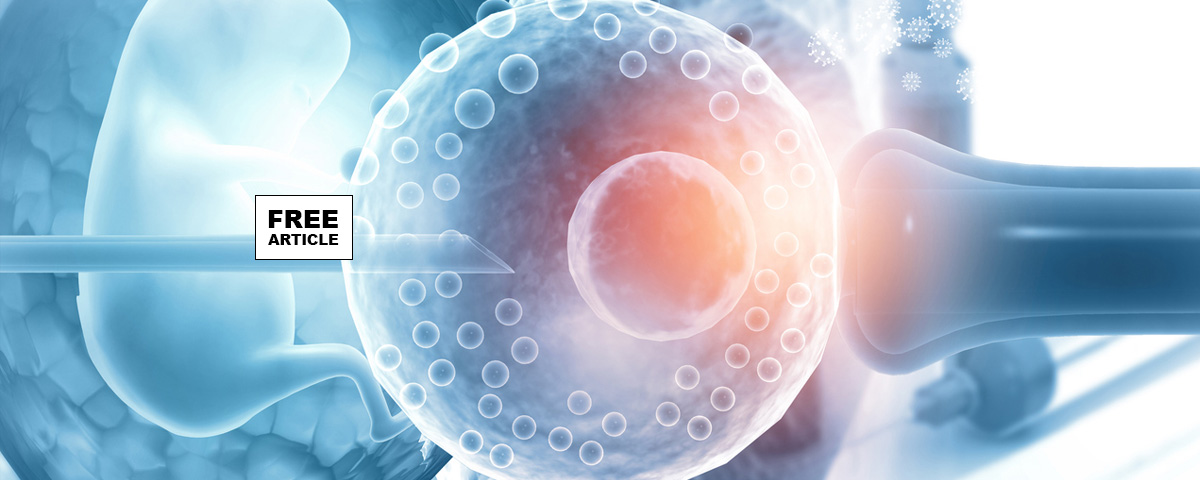
In the journey of assisted reproductive technology (ART), in-vitro fertilization (IVF) has emerged as a transformative solution for individuals and couples striving to achieve parenthood. Among the various techniques in IVF, Frozen Embryo Transfer (FET) has gained remarkable prominence. Frozen Embryo Transfer, FET involves the cryopreservation of embryos and their subsequent thawing and transfer during a later menstrual cycle. Over the years, FET has demonstrated significant advantages, particularly in yielding higher implantation and pregnancy rates as compared to fresh embryo transfers. This article explores how FET has evolved, the scientific rationale behind its success, and its implications for reproductive medicine.
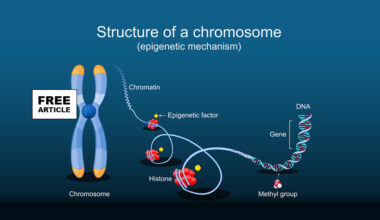
Cryopreservation involves freezing embryos at sub-zero temperatures using vitrification—a rapid freezing technique that reduces the risk of ice crystal formation, which can damage the embryo’s cellular structure. The embryos remain in suspended animation until the woman is ready for the transfer. Vitrification has significantly improved FET outcomes by maintaining high survival rates for thawed embryos.
In traditional fresh embryo transfer, embryos are transferred during the same cycle in which ovarian stimulation and egg retrieval are performed. However, ovarian stimulation can significantly alter the uterine lining, the endometrium, potentially reducing its receptivity to the embryo. FET offers a solution by allowing the body to recover from the hormonal impact of stimulation, thus creating a more natural and favorable uterine environment for implantation.
Several studies and clinical trials have demonstrated that FET results in higher implantation and pregnancy rates compared to fresh transfers. This success can be attributed to multiple factors:
A key reason for higher implantation rates in FET cycles is the improved receptivity of the uterine lining. Hormonal stimulation during fresh IVF cycles can disrupt the natural synchronization between the embryo and the endometrium. In contrast, during FET cycles, the uterus is often in a more natural state, free from the hormonal disturbances caused by ovarian stimulation.
Advances in vitrification have contributed to the high survival rates of frozen embryos post-thawing. Research suggests that embryos that survive the freezing and thawing process are often robust and possess greater developmental potential. This resilience translates into higher implantation success.
Ovarian Hyperstimulation Syndrome OHSS is a potential risk during IVF treatments, particularly in cases of fresh transfer cycles. By opting for FET, patients can minimize the risk of OHSS, as the transfer occurs in a cycle separate from ovarian stimulation.
FET also allows clinicians to better control the timing of the embryo transfer, ensuring that the uterine lining is optimally prepared and synchronized for implantation. This precision is especially advantageous for patients with irregular cycles or other complications.
Numerous studies have highlighted the success of FET in achieving higher pregnancy rates. For example, a meta-analysis comparing fresh and frozen embryo transfers concluded that frozen transfers were associated with a higher live birth rate. Similar findings have been observed across various demographics and age groups, reinforcing FET as a preferable option in many cases.
Additionally, FET has been linked to a reduced likelihood of multiple births. By transferring embryos in a more controlled and strategic manner, clinicians can encourage single embryo transfers, thereby reducing the risks associated with twins or higher-order pregnancies.
FET has also shown promising results for patients with specific conditions, such as polycystic ovary syndrome (PCOS), where ovarian stimulation may adversely affect fresh transfer outcomes. Similarly, for patients undergoing preimplantation genetic testing, FET provides an optimal solution by allowing time for genetic analysis without rushing the transfer process.
While FET has revolutionized IVF, it is not without challenges. The process of freezing and thawing requires expertise, and not all embryos may survive the process. Additionally, the success of FET depends on the careful preparation of the uterine lining, which may require personalized hormonal treatments.
The advent of frozen embryo transfer has transformed the landscape of assisted reproductive technology. By offering higher implantation and pregnancy rates, FET has become a cornerstone of modern IVF practices. Its advantages, ranging from improved uterine receptivity to reduced health risks, make it a compelling choice for many patients. As technology and research continue to evolve, FET is poised to further elevate the success of IVF, bringing the dream of parenthood closer to reality for countless couples around the world.