Preterm birth is defined as any birth that occurs before 37 weeks of gestation and is the leading cause of illness and death among newborns. The 2023 March of Dimes Report Card reveals that more than one in ten infants were born prematurely in the United States in the past five consecutive years and for the third consecutive year, the March of Dimes Annual Report Card has given the United States a D+ for the country’s persistently high preterm birth rate.
Prematurity is linked to a significantly elevated risk of major long-term medical complications, such as learning disabilities, cerebral palsy, chronic respiratory illnesses, intellectual disabilities, seizures, and vision and hearing loss. It can also lead to substantial costs throughout the lives of affected children. The annual healthcare expenses for managing the short- and long-term complications of prematurity in the United States alone were estimated to be around $25 billion for 2016.
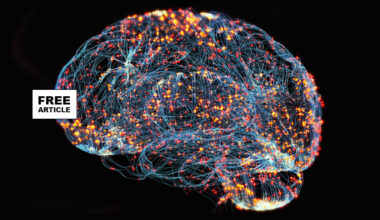
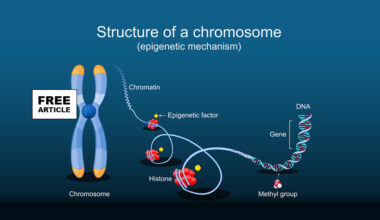
The PreTRM® Test is a commercially available blood-based biomarker test that provides an early, accurate, and individualized risk prediction for spontaneous preterm birth in asymptomatic singleton pregnancies. The PreTRM® Test measures and analyzes proteins in the blood that are highly predictive of preterm birth.
A multicenter randomized controlled trial was conducted in 5,018 pregnant women at low risk for preterm birth in 19 centers across the United States. Individuals with factors that increase the risk of preterm birth — such as a prior preterm birth, a short cervix, multiple gestations, or severe medical conditions such as lupus or chronic renal disease — were excluded from the trial, thus allowing the researchers to examine the low-risk population.
The biomarker test, which analyzed a participant’s blood, was administered in the middle of the second trimester of pregnancy to identify individuals at higher risk of delivering an infant preterm. The test classified 23.5 percent of participants as higher risk within the preterm birth prevention arm. In addition to the traditional standard of care, individuals identified as high risk were given a regimen of daily vaginal progesterone and low-dose aspirin and also assigned weekly standardized phone calls with a nurse. The remaining lower-risk participants received the usual standard of pregnancy care, which included routine checkups.
In the preterm birth prevention group that was screened and treated if the mother had a higher risk test result, data showed a 20 percent reduction in neonatal morbidity and a 20 percent reduction in Neonatal ICU admissions. Results also further demonstrated that infants admitted to the neonatal ICU had a 6-8 percent reduction in the length of stay.
This study is the first to combine a biomarker test that screened a large segment of the population who did not have the typical risk factors for preterm birth with a targeted treatment plan for those who were identified to be at higher risk with the test and demonstrated dramatic improvements in neonatal outcomes. These findings suggest a transformative strategy for reducing neonatal complications and has the ability to change the practice of obstetrics and prevent neonatal issues associated with preterm birth.
If you are interested contact your physician.