Cardiovascular disease (CVD) affects 6.6 million women in the United States annually and is the leading source of morbidity and mortality among women. Among women diagnosed with cardiovascular disease, 2.7 million have a history of MI – Myocardial Infarction (heart attack). Each year more than 53,000 women die of a heart attacks and 262,000 are hospitalized because of CVD. One in 4 female patients presenting with a first myocardial infarction will die.
Cardiovascular disease (CVD) in women remains under-diagnosed and undertreated due to the diagnostic challenge it presents, as well as the persisting attitude that CVD predominantly affects men. Gender-related risk factors have now been identified but there is a lack of clinical application, leading to the misdiagnosis and poor management of women with CVD.
Anatomically, women have smaller hearts even after adjustment for body size, and, as a result, have different disease phenotypes (observable characteristics), which may influence the choice and accuracy of diagnostic tests. Further, there are intrinsic imaging difficulties with standard transthoracic echocardiography in women due to reduced image quality from breast tissue attenuation and reluctance to use cardiac computed tomography (CCT) in pre-menopausal women due to breast tissue sensitivity.
Women present with ischemic heart disease about a decade later than men. This usually occurs in the postmenopausal period, during which time the protective effects of estrogen are attenuated. Furthermore, population-based risk reduction in women has not resulted in improvements in the incidence of CVD compared to men. In recent years, there has been a significant decline in the incidence of myocardial infarction (MI) in men, and a comparative increase in the incidence in older women. Further evidence supporting this finding from the National Health and Nutrition Examination Surveys demonstrated an increase in the prevalence of Myocardial Infarctions in women in the 35–54-year age range, while a decline in prevalence was observed in age-matched men. It follows that early and accurate diagnosis of CVD is pivotal to reduce mortality rates in women.
Women share many traditional risk factors with men such as smoking, high lipid levels and diabetes. However, they also have sex specific risk factors including pregnancy-related complication such as preeclampsia, gestational diabetes, and pre-term birth all of which increase future cardiovascular risk. Menopause and the loss of estrogen’s cardioprotective effect also increase CVD risk. Autoimmune diseases like lupus and rheumatoid arthritis are more common in women and further increase the risk of cardiovascular disease. Comon disorders of young women like Polycystic Ovary Syndrome are associated with obesity, diabetes and metabolic syndrome also cause an increased lifetime risk of CVD.
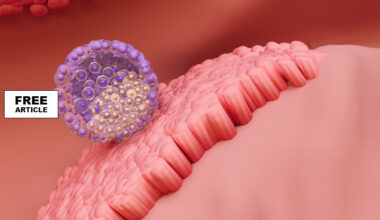
Cardiovascular disease in men is very different often leading to diagnostic confusion since the male model is routinely used as the paradigm of CVD. Men are more likely to have obstructive CVD specifically, large plaques causing blockage of the large coronary arteries. Women on the other hand are more likely to have microvascular disease and plaque erosion. There is over-representation of women with MI (heart attack) with Non-Obstructed Coronary Arteries (MINOCA) relative to those with elevated troponin (a protein marker of cardiac damage) resulting from obstructive Coronary-Artery-Disease (CAD) Only 24–30% are women present with obstructive CVD. Mechanisms of MINOCA that are more commonly observed in women include coronary microvascular dysfunction and coronary artery plaque erosions.
New and more sophisticated diagnostic testing should be made universally available for women to more accurately diagnose underlying CVD and prevent unnecessary morbidity and mortality.
Sources
https://jcmr-online.biomedcentral.com/articles/10.1186/s12968-020-00666-4
https://www.sciencedirect.com/science/article/abs/pii/S0095454317301318
https://pmc.ncbi.nlm.nih.gov/articles/PMC4834856/
https://www.heartlungcirc.org/article/S1443-9506(20)30280-8/fulltext