Nature protects you and your child by selecting only the best embryos so that you have the best chance of giving birth to a healthy child. This article will explain the natural selective process and its protective function. Perhaps more importantly we will suggest strategies that can help increase your odds of having a healthy child. One Strategy is egg freezing or embryo banking to ensure you have a young healthy egg available if you are not ready to have a child yet but want to keep your options open. The other is IVF where the embryologist selects only the highest quality embryos.
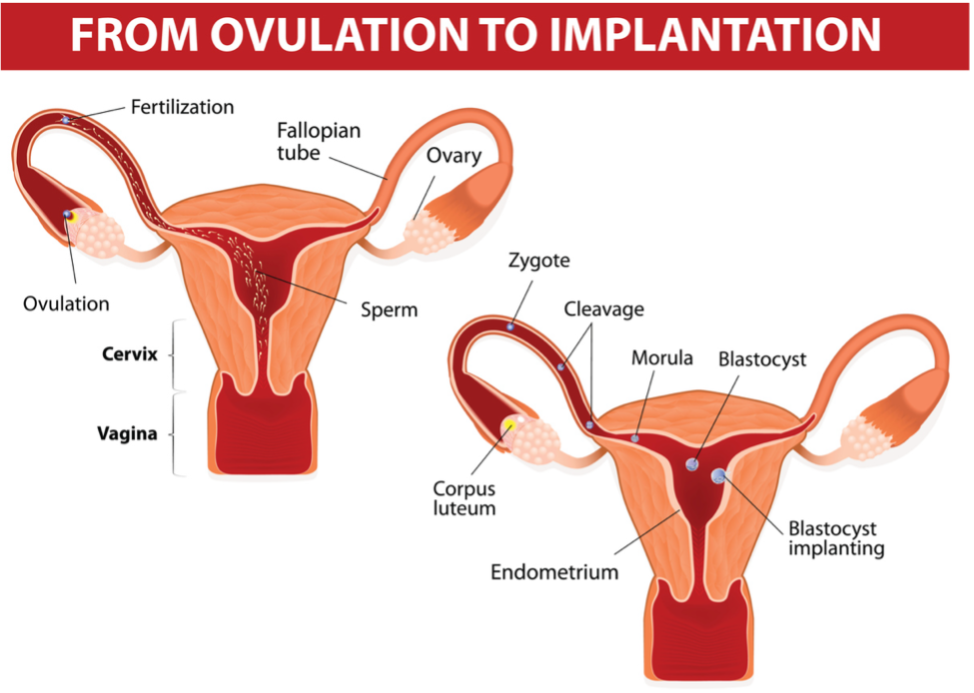
Conception:
After traversing the cervix and reaching the fallopian tube sperm can fertilize an egg. Fertilization is the process by which male and female gametes fuse to form a zygote (a unicellular structure with a complete set of 46 chromosomes). Fertilization usually takes place in the ampulla, the widest part of the fallopian tube, 12 to 24 hours after ovulation. After this period of time, the egg loses its ability to be fertilized and begins to degenerate. When the egg is fertilized and a zygote is formed, cell division begins with the embryo reaching the uterus about 3-4 days later at what is called the morula stage when the embryo is seen as a solid ball of cells. On day 5 or 6 a blastocyst, a hollow ball of cells is formed and subsequently implants in the endometrium, the lining of the uterus, on day 6 or 7. This is the first stage of pregnancy. Pregnancy can be detected at this stage because after implantation the hormone Human Chorionic Gonadotropin (HCG) is produced by the embryo’s trophoblast cells (cells which will later become the placenta) and enters the mother’s bloodstream and urine. Detection of the HCG from the embryo that has entered the mother’s bloodstream, and urine is the basis of pregnancy tests. At this early-stage pregnancy is not normally detected on an ultrasound. Hence, the reason for the blood and urine tests.
Two-thirds of all human pregnancies are lost. It has been estimated that a large proportion of pregnancies are lost shortly after the implantation stage before the pregnancy is clinically recognized. These very early losses that occur before an embryo has fully developed are assumed to be due to structural malformations or chromosomal aberrations, incompatible with further development and life. Chromosomal abnormalities are found in 60% of pregnancy losses and only 0.1% of live births and are the most common cause of pregnancy loss. This is natures selective way of preventing fetal abnormalities. With few exceptions only embryos devoid of chromosomal abnormalities will become healthy babies. Nature protects the species.
The risk of pregnancy loss is affected by reproductive history and is greatest in the older age groups. Evidence suggests that this risk follows the rate of aneuploidy. Aneuploidy is defined as a condition where a cell has an abnormal number of chromosomes. Instead of having the typical number, 46 – 23 from each parent a zygote or embryo with aneuploidy may have one or more extra chromosomes or be missing one or more chromosomes. The highest rates are observed for mothers under the age of 20, and those older than 33. This is consistent with the fact that current estimates of chromosomal abnormalities in pregnancy losses are higher than reported in earlier studies, probably because a greater proportion of women are now conceiving at advanced maternal age. Thus, not surprisingly, the majority of chromosomal abnormalities are maternally transmitted.
In addition to the large number of pregnancies that are lost shortly after the implantation stage even before the pregnancy is clinically recognized, an additional, 10% to 20% of clinically recognized pregnancies will end in early pregnancy loss. However, these statistics likely underestimate the true incidence of spontaneous loss, as many miscarriages remain undiagnosed, with the resulting bleeding being mistaken as heavy, late menses. Studies that have tracked pregnancies using daily measurements of serum HCG levels estimate a higher incidence of approximately 38%. Additionally, 12% to 57% of pregnancies with first-trimester bleeding end in miscarriage. In more than 60% of pregnancy losses between 6 to 10 weeks of gestation, the cause is believed to be fetal chromosomal abnormalities, including trisomy where a fetus has 3 copies of a particular chromosome rather than 2 for a total of 47 rather than 46, monosomy where the fetus is missing one chromosome of a normal pair or a total of 45 rather than 46, and polyploidy where multiple extra chromosomes are seen. Additionally, inflammatory and immunologic dysregulation is thought to play a role in some cases.
The most common risk factor for early pregnancy loss is advanced maternal age. For example, the incidence of early pregnancy loss in women aged 20 to 30 years is only 9% to 17%, while the incidence at 45 years of maternal age is 75% to 80%. A prior history of pregnancy loss also increases the risk of recurrent pregnancy loss, with the risk increasing after each additional loss. For example, the risk of miscarriage in a future pregnancy is approximately 20% after one miscarriage, 28% after 2 consecutive miscarriages, and 43% after ≥3 consecutive miscarriages. Additionally, first-trimester vaginal bleeding, which occurs in up to 25% of pregnancies, is associated with a higher risk of pregnancy loss.
Fertility preservation via egg freezing when parenthood is not feasible or desirable at the present time is a viable option to minimize the risk of pregnancy loss. A woman is born with all the eggs she will ever have. Eggs released when a person is younger are most often of better quality and more likely to result in a healthy pregnancy. Egg freezing or embryo banking allows people to preserve their fertility at their current age and then try to become a parent when they are ready, reducing the risk of pregnancy loss. As noted above advancing age is correlated with the risk of pregnancy loss. The age of a pregnancy is not related to the age of the women but rather the age of the egg. A 40-year-old woman who uses eggs frozen at age 28 will have the same pregnancy loss risk as a 28-year-old.
IVF offers the best opportunity for a healthy pregnancy because the embryologist can select a blastocyst that has the best chance of creating a successful pregnancy. Unfortunately, unlike the rest of the civilized world which has universal insurance coverage for IVF only 15 U.S. states and the District of Columbia have passed fertility insurance coverage laws that include IVF. This is a great disservice to American women and their families and puts the lie to those who claim to support women’s reproductive rights. Abortion, the right not to have a child is of course important but it seems paramount to these advocacy groups since, little or no effort is made to protect the rights of women who may have medical issues that preclude a natural pregnancy but still wish to have a child.
https://www.nature.com/articles/s41594-023-01209-y