Premenstrual Syndrome (PMS) is a common disorder affecting women of reproductive age. Many women experience dysphoria and physical symptoms approximately two weeks before menstruation. The discomfort, both physical and psychological, is associated with the luteal phase, the second half of the menstrual cycle, and typically resolves when menstruation ends. The global prevalence of premenstrual syndrome is estimated at 47.8%, while the most severe form of PMS – Premenstrual Dysphoric Disorder (PMDD) affects 3-8% of women of reproductive age. The most common psychological symptoms of PMS include irritability, tearfulness, anxiety, and depressed mood. Physical ones, on the other hand, mainly involve abdominal bloating, breast tenderness, and headaches.
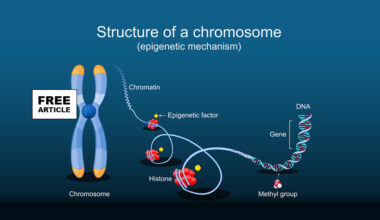
The cause of PMS is intricate and not completely understood. Several theories attempt to explain the causes of its symptoms. Classically, PMS has been linked to hormonal fluctuations during the monthly cycle, with mood deterioration and increased anxiety primarily associated with decreases in estrogen and progesterone. Recently, a great deal of attention has been given to a breakdown product of progesterone, allopregnanolone. Allopregnanolone is modulator of the GABA receptor in the Central nervous system, CNS. Allopregnanolone binds to the GABA receptor which explains its broad effects on multiple Central Nervous System, CNS pathways. Moreover, allopregnanolone synthesis can occur de novo not only in the brain but also in the ovaries and adrenal glands due to the presence of necessary enzymes in these organs needed for its production. Understanding the significance of allopregnanolone in alleviating PMS symptoms may provide crucial information about the cause of the disorder itself. Due to these associations and the increased interest in neuro-steroids, allopregnanolone has become one of the most linked substances to the cause of PMS in recent years.
Women experiencing premenstrual symptoms demonstrate an impaired stress response. This may be linked to the action of the steroid hormones’ estrogen and progesterone which, through various mechanisms, inhibit the activity of the Hypothalamic Pituitary Axis (HPA axis) starting at the Paraventricular Nucleus of the Hypothalamus. Progesterone, or more specifically, its breakdown product — allopregnanolone, enhances GABA conductance and suppresses Corticotropin-releasing hormone CRH formation in hypothalamic cells. CHR is a central player in orchestrating the body’s response to stress.
In contrast, estrogen normally inhibits the generation of free radicals, resulting in a reduction of oxidative stress in the body and would help ameliorate PMS. It has been suggested that abnormal oxidative and inflammatory activity may occur in PMS. It is possible that in PMS, there is an abnormal response to estradiol and an increase in oxidative stress. This is significant because there is normally a second peak in estrogen in the luteal phase, the second half of the menstrual cycle when PMS occurs which if working properly should tend to reduce the risk of PMS symptoms.
Interestingly, there are no discernible differences in hormone levels during the monthly cycle between healthy women and those suffering from PMS. However, concentrations of allopregnanolone and its conversion from progesterone are higher in women with PMS and PMDD. This suggests a disturbance in the metabolic pathway of progesterone in women who are affected and implies the existence of a subgroup of women sensitive to hormone. Furthermore, the importance of allopregnanolone was demonstrated in a recent study that showed that women with PMS who toke a drug that blocks 5-alpha-reductase, a crucial enzyme for allopregnanolone production, experienced significantly reduced premenstrual symptoms.
Genetics plays a role in PMS. Family studies suggest a discernible genetic component and align with the theory of the existence of a subgroup of susceptible patients. Research conducted found that children of mothers with PMS have a higher likelihood of developing the disorder. Additionally, a study on identical and fraternal twins highlighted a greater than 40% probability of developing the disorder if one of the twins suffers from PMS.
The most effective drug in the oral contraceptive (OC) group seems to be formulations containing ethinyl-estradiol and drospirenone. This preparation is FDA-approved for the treatment of PMDD. These drugs are intended to improve the patient’s condition through several mechanisms, including the suppression of ovulation, which results from the stabilization of hormone levels by both components of the pill. Theoretically, this is also expected to lead to an improvement in mood. The preparation is also intended to have an anti-androgenic effect, which would reduce symptoms such as irritability and aggression. However, the role of androgen hormones in PMS is not yet fully understood.
Although traditional oral contraceptive OC treatment is effective, it does not fully eliminate hormonal fluctuations. This may be related to a treatment regimen involving 7 days a cycle without any hormones. The use of COC – continuous contraception – could eliminate LH, FSH, estradiol, and progesterone fluctuations, thus improving patient comfort. A recent trial studied the effectiveness of levonorgestrel 90 mcg/ethynyl estradiol 20 mcg for 4 cycles of 28 days. The study found that over half of the patients experienced a significant improvement, defined as a 50% reduction in symptom intensity.
The use of oral contraceptives that contain only progesterone is not recommended for the treatment of PMS and PMDD symptoms. This is because such therapy may exacerbate mood fluctuations and other PMS-related symptoms via the production of the allopregnanolone metabolite.
Alongside oral contraceptives, gonadotropin-releasing hormone (GnRH) agonists also play a significant role in the treatment of PMS and PMDD. The mechanism of action involves inhibiting the central hypothalamic-pituitary-ovarian system, which leads to the inhibition of ovulation. Given the adverse effects of these agents, they should probably be reserved for very severe cases.
In summary, PMS therapy with oral contraceptives containing drospirenone and ethinyl estradiol (at a dose of 3 mg drospirenone and 20 mcg ethinyl-estradiol) are the most effective. If bleeding and abdominal pain are not controlled, an alternative solution is to use continuous contraception COCs with levonorgestrel and ethinyl-estradiol. Transdermal patches may be used as an alternative to oral contraceptive pills for patients who have difficulty taking them regularly. However, the effectiveness of transdermal patches is still a matter of debate. It is not recommended to use formulations that contain only progesterone. The available research on the effectiveness of new treatments that selectively target progesterone, and its metabolites is insufficient to draw firm conclusions. However, this could be the future of PMS therapy.
It is important to note that many PMS and PMDD symptoms, including breast tenderness, depression, and headaches, can occur as side effects of taking contraception, which limits the effectiveness of this approach. Although side effects were rare in most studies.
Source
https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2024.1363875/full